AAFP physician happiness survey results
In fact, only 61 percent of respondents said they’d become physicians if they could do it over again — which means a full 39 percent of practicing physicians would consider a different path if they could start over. This should give hospital administrators pause, especially when considering what causes unhappiness among physicians. By addressing these pain points and stressors, administrators can increase the satisfaction of their physicians and improve retention.
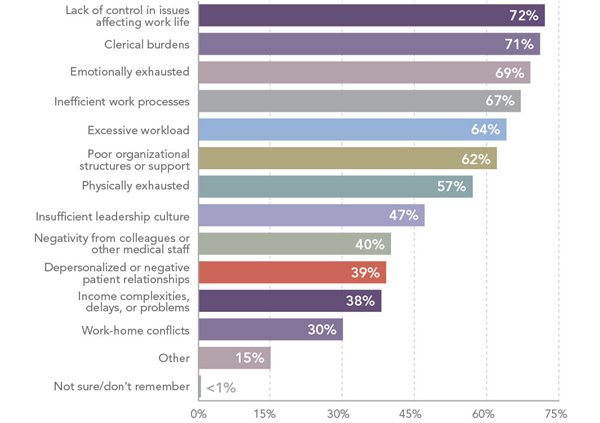
Factors leading to unhappiness
The top factor leading to discontentment among physicians is a lack of control over their work. A hefty 72 percent of respondents cited a lack of control or autonomy as leading to unhappiness – and only 13 percent reported having full control over their work. Physicians long for autonomy, and administrators should consider developing a leadership approach that empowers physicians wherever possible.
The second-greatest cause of unhappiness at 71 percent is clerical burdens, which add to an already-substantial workload and pull physicians away from time spent with patients. On average, physicians reported working 10 hours per day, with only 68 percent of that time spent with patients. Reducing patient loads and relieving clerical duties wherever possible can help physicians feel more engaged with their patients — and less burnt out.
While 68 percent of physicians said they have the resources they need to perform their jobs efficiently, only 31 percent felt their organizations prioritized their well-being — a figure that should sound alarm bells for administrators. The following chart highlights the key reasons for physician unhappiness.
Need for recognition
Sometimes a simple pat on the back can go a long way, but only 34 percent of physicians said they felt appreciated for their work, and only 29 percent had ever been formally recognized. These numbers aren’t great — but they do suggest an opportunity to improve morale by developing a formal recognition program, as well as spontaneous, heartfelt expressions of appreciation.
When physicians do receive formal recognition, they tend to receive it from patients (40 percent), peers (33 percent), and students (26 percent). Adding formal recognition from the health care organization can help physicians feel a deeper sense of appreciation for their work.
Workplace friendships and mentors
One positive factor impacting physician happiness is friendships. The study suggests a direct correlation between the number of friends physicians have at work and satisfaction with their lives. Of those who reported having many friends at work, 70 percent also reported high life satisfaction. On the other hand, of those who said they had no friends at work, only 39 percent had high life satisfaction. Similarly, 69 percent of those who had many friends said their colleagues were supportive, while only 29 percent of those with no friends felt supported.
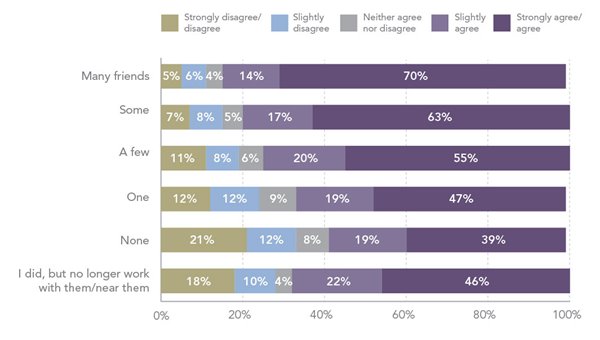
The vast majority of physicians, at 84 percent, reported having positive relationships with their peers. But when asked about their relationships with administrators, only 50 percent described those relationships as positive. It seems clear that it’s vital to foster a workplace culture that encourages physician friendships and works to build strong relationships between physicians and administrators.
In addition to workplace friendships, strong mentoring relationships were important to physicians. Fifty-two percent of physicians said mentors have been very or extremely important to their careers, and 73 percent of them have served as a mentor, either formally or informally — while another 18 percent would like the opportunity to mentor.
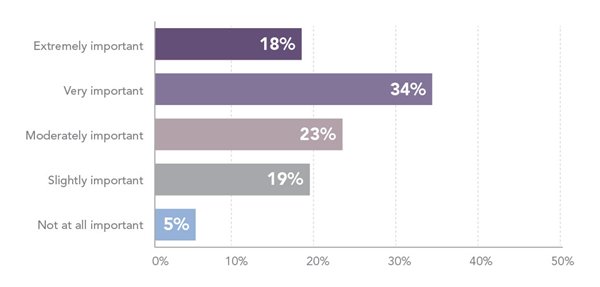
As these relationships seem important both to the mentor and the mentee, health care organizations should find ways to encourage mentorships through formal programs, as well as informal relationships.
Bottom line: The majority of physicians are happy and satisfied with their lives. But a large undercurrent of stress and discontentment remains, giving health care organizations a real opportunity to improve physician happiness and retention. The place to start is in prioritizing physician well-being, and then fostering a culture that recognizes contributions, encourages friendships, and supports mentoring.
This article originally appeared on CompHealth.com, a trusted NRHA partner, for publication within the Association’s Rural Health Voices blog
