Guarding the heart of rural health care: Addressing workplace violence
Workplace violence is a growing risk in hospitals. Reported incidents seem to be everywhere. Proactive attention to this matter is important, and taking actionable steps now will benefit your organization if and when an incident occurs.
The term “workplace violence” is described by the National Institute for Occupational Safety and Health as “any physical assault, threatening behavior, or verbal abuse occurring in the work setting.” It’s a problem that is not specific to urban areas. Rural health care facilities are experiencing serious incidents as well. One such event occurred in Tell City, Ind., where a police officer and a suspect were killed in a shootout in front of a hospital last summer.
 |
The impact of workplace violence on health care is serious. How an organization prepares for and responds to workplace violence can affect staffing, recruitment, staff burnout, employee stress and anxiety, and the community. It’s an important issue to understand, mitigate, and prepare for when considering the safety of your hospital environment.
Planning for an unthinkable act
We face many risks in health care facilities. We write disaster plans for electrical outages, natural disasters, and patient influx. We can follow similar steps when planning for a workplace violence incident. Consider how health care has approached fire safety:
- Planning: Facilities are designed and built to prevent fires and protect the occupants if a fire occurs. A risk assessment helps identify vulnerabilities in staff knowledge and building systems.
- Preparedness: Under the organization’s fire response plan, employees are trained to respond to a fire, protect vulnerable patients, and protect themselves. Fire drills are routinely scheduled to test and educate staff on how to “do it right.” Mitigative measures – such as fire extinguishers, fire alarm systems, and fire sprinkler systems – reduce risk.
- Response: Because of planning and preparedness, fires are rare. Staff respond well when there is a fire, and impact and injury have dramatically improved.
- Recovery: Our ability to return to normal operations and continue to care for our community, employees, and patients has improved.
 |
This same approach can work for workplace violence prevention.
- Assemble a team to bring focus to the problem. The risk assessment and gap analysis will need different perspectives from within the organization. The team might include people responsible for security, employee health, risk management, and facilities management, along with clinical staff. Some organizations may also have a patient advisory council.
Listening to hospital staff provides perspective on potential blind spots that leadership is unaware of. Addressing staff-identified concerns will also nurture trust that valid concerns are being addressed. - Perform a risk assessment and a gap analysis. Include exterior and interior portions of the building. This would involve identifying hospital areas that may be more at risk, such as parking areas or an emergency department.
The risk assessment for health care security should be more granular to identify specific portions of a department, certain processes that tend to have a higher risk, certain times of day and days of the week, or specific community events.
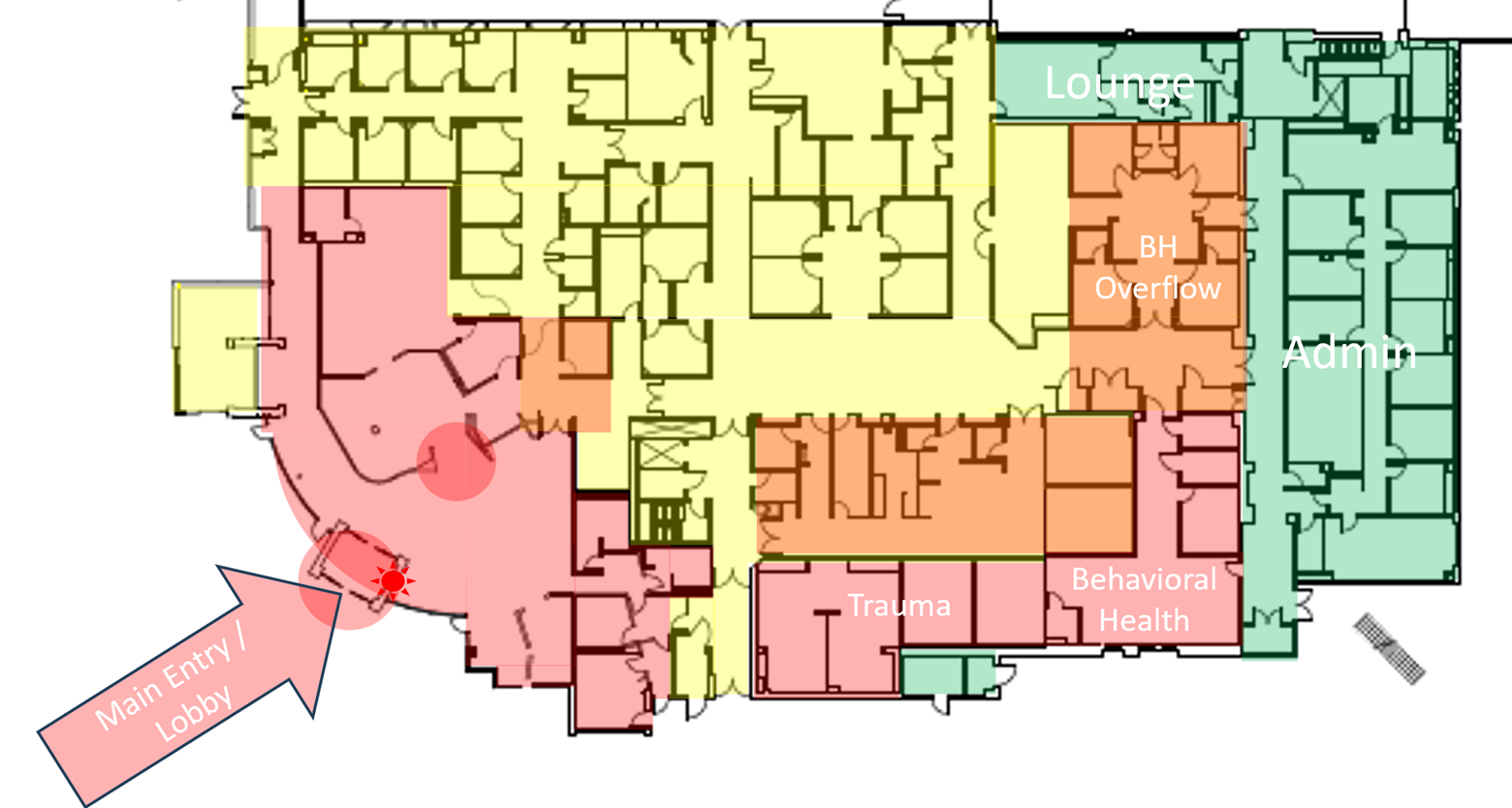
A useful visual tool could be a “heat map.” This is an illustration using the floor plan of a unit or a building to indicate where higher-risk areas are located. In this example of an emergency department, the organization identified the main entry and intake area as the highest risks for workplace violence. Portions of the department used for trauma or behavioral health were also considered high risk. - Identify and implement mitigation measures. Mitigation takes many forms. Static measures might include improving lighting in parking areas and entry points to the building. Staff education and training are active measures, particularly in areas at higher risk, and such training can help staff deescalate risky situations.
Security presence is often an effective mitigation measure. The visibility and mobility of recognizable security forces reassure staff, patients, and visitors. For rural hospital safety, encourage relationships with local law enforcement or in-house security personnel, and make rounding and interaction with clinical staff a routine.
Though training and preparation are beneficial, they are not without risk. Leadership should recognize that performing workplace safety exercises may pose psychological risks to staff, particularly in realistic scenarios. - Develop a response plan. Workplace violence incidents tend to be short in duration, comparable to fire drill response. Understand that there is little time to assemble a command staff, because the event will likely be over when an incident command activates.
Although response is critical, it is important to recognize that the command-and-control effort will be complex due to the rapid development of the situation and the confusion that results from it. - Develop a recovery plan.Much of your focus will be on recovery efforts. The recovery impacts may last weeks and could include:
- Injuries to staff, patients, or visitors that continue to need attention.
- Crime scene security and law enforcement gathering of evidence.
- Traumatic impact on staff that may last days or weeks.
- Staffing challenges.
- Community mourning.
 |
Workplace violence can occur at many levels that we need to prepare for in similar ways. Beyond an active shooter or a violent physical assault within the hospital, other instances could include:
- An abusive patient disputing a bill.
- A nurse being assaulted in a parking area.
- A home care nurse being mugged while on a home visit.
- Verbal and emotional abuse between coworkers.
- An angry patient or family member targeting a provider.
Workplace violence is a pervasive issue that demands our attention and action. As evidenced by incidents like the shootings in Indiana, no workplace is immune, including rural health care facilities. The repercussions of workplace violence extend beyond physical harm, affecting staffing, recruitment, employee well-being, and community trust. By adopting a systematic approach akin to fire safety planning with robust response and recovery plans, health care organizations can better prepare for and mitigate these risks.
NRHA adapted the above piece from the Accreditation Commission for Health Care, a trusted NRHA partner, for publication within the Association’s Rural Health Voices blog.
 | About the author: Richard Parker, MBA, spent five years as a life safety surveyor for Accreditation Commission for Health Care Inc. (ACHC) hospitals before transitioning in August 2022 to the role of associate director for life safety and physical environment, providing oversight for these areas and for emergency management requirements across accreditation programs. |
