Helping rural hospitals strengthen payer negotiations
Rural and critical access hospitals operate in uniquely challenging environments, often managing narrow margins, shifting patient volumes, and evolving pressures from payers. In this landscape, visibility into how services are reimbursed across the market is critical but often difficult to obtain.
The conversation around health care price transparency gained momentum after two major federal mandates were introduced:
- Hospital Price Transparency Rule (effective Jan. 1, 2021): This rule requires hospitals to publish standard charges for services, including negotiated rates with payers.
- Transparency in Coverage Rule (effective July 1, 2022): Requires payers to publish the reimbursement rates they have with health care providers.
What this means and why it matters
While the Hospital Price Transparency Rule focuses on what hospitals charge and what patients may pay, the Transparency in Coverage Rule goes a step further, requiring commercial payers to publish what they actually reimburse providers. This gives rural hospitals access to real negotiated rates at the CPT and plan level across markets and competitors.
Together, these regulations have opened the door to a massive amount of previously hidden data. For rural hospitals, this payer-level data offers a powerful opportunity to gain visibility into how services are reimbursed, benchmark rates across regions, and potential underpayments, allowing them to approach negotiations with clearer context and greater confidence.
When used strategically, this insight can help strengthen payer relationships, improve operating margins, and support long-term access to care.
Use cases for price transparency data in rural strategy
When paired with the right tools, price transparency data becomes more than a spreadsheet — it becomes a decision-making framework. Below are five key ways rural hospitals can apply this data to strengthen their strategy.
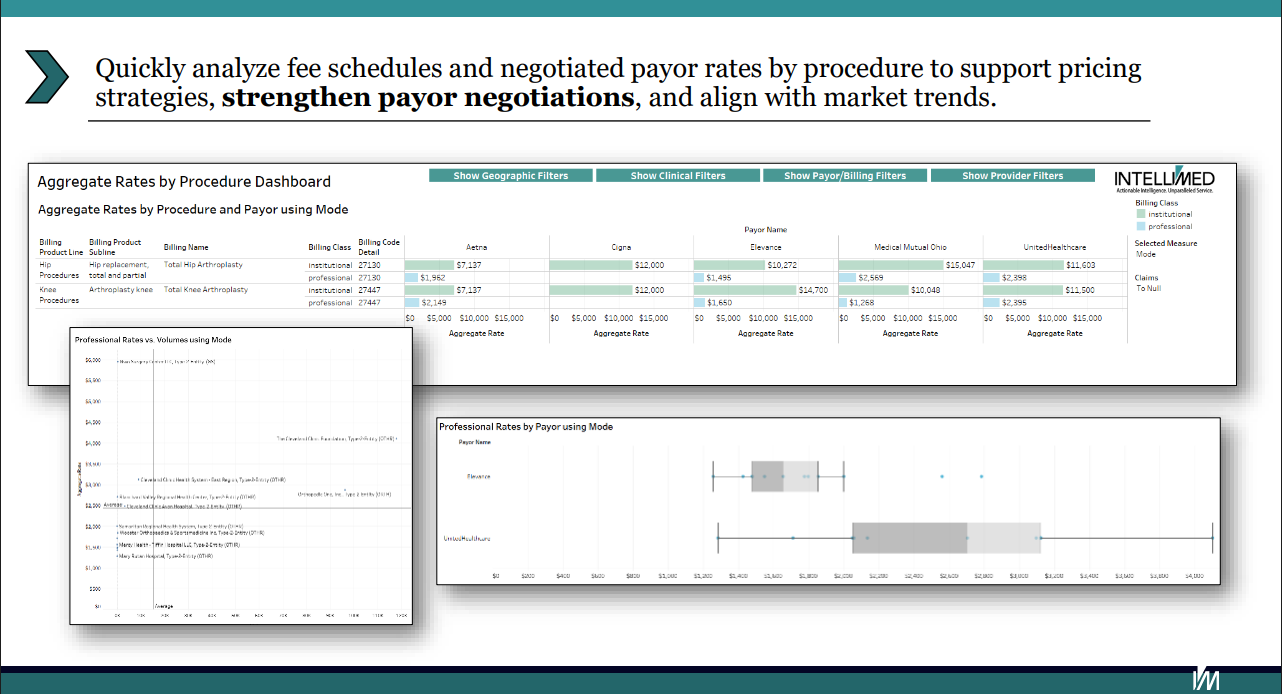
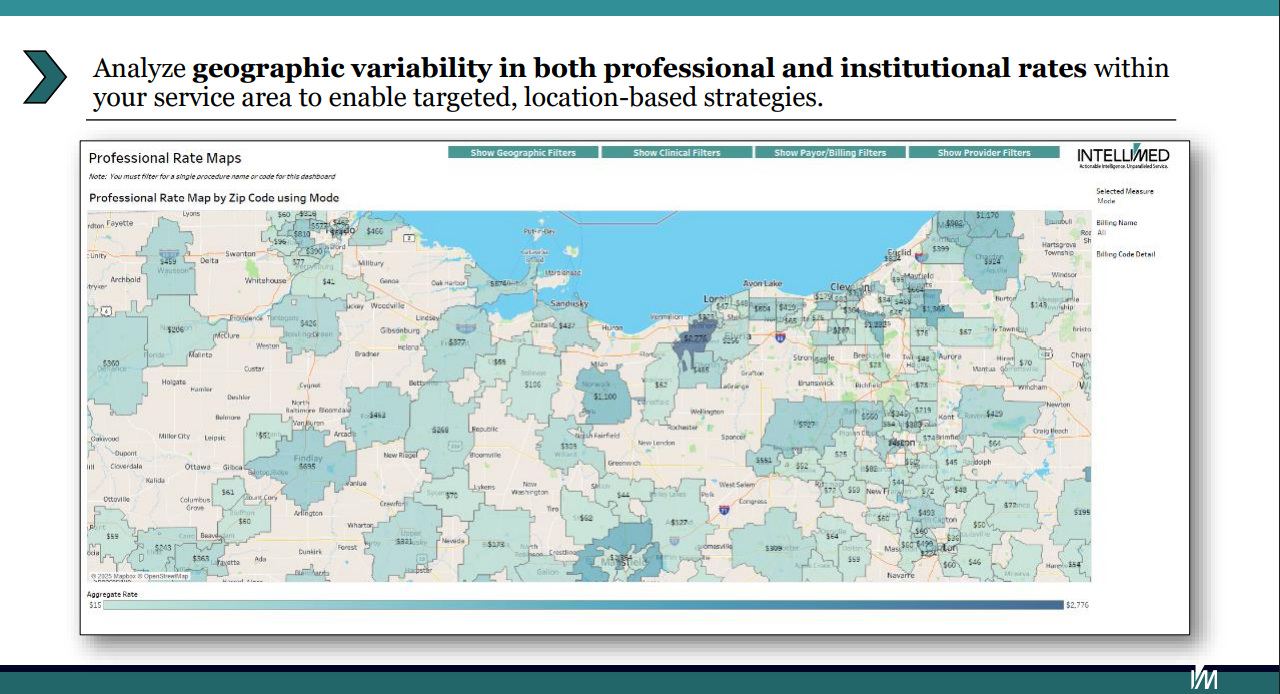
1. Market benchmarking for strategic negotiations
Use reimbursement rate comparisons across facilities and regions to:
- Assess your organization and provider-specific negotiated rates against market standards
- Pinpoint where your facility may be under- or over-reimbursed
- Strengthen negotiation positions by demonstrating market-driven rate expectations
Benchmarking helps rural hospitals advocate for competitive reimbursement that reflects their value to the community and the payer.
2. Strengthen payer contracting strategies
Leverage detailed rate insights to:
- Enhance managed care contract negotiations
- Ensure competitive positioning in your market by aligning rates with broader trends
- Link reimbursement data with provider utilization trends to prioritize rate adjustments
Data-backed negotiation strategies help hospitals secure more sustainable contract terms.
3. Develop value-driven provider networks
Identify and assess providers based on reimbursement rates to:
- Design high-value, cost-efficient provider networks
- Target partnership opportunities with providers and group practices delivering strong outcomes and favorable reimbursement profiles
- Support network development that balances patient access and financial sustainability
This approach supports both referral strategy and value-based care initiatives.
4. Quantify service line growth opportunities
Analyze reimbursement patterns across specialties to:
- Inform service line development plans and service expansion strategies
- Pinpoint services with high demand and favorable reimbursement rates
- Support revenue projections tied to specific payers and procedures
This enables rural hospitals to grow strategically, aligning investments with financial opportunity.
5. Calculate comprehensive cost of Care
Combine facility and provider rates to:
- Evaluate the true cost of care delivery across different services and populations
- Identify areas where operational efficiency or pricing adjustments can drive improved margins
- Support strategic financial planning and resource allocation
Understanding the full cost landscape strengthens long-term sustainability initiatives.
Turning payer price transparency data insights into action
Price transparency data opens the door for rural hospitals to better understand their position in the market — but it’s how that data is used that ultimately drives impact.
Hospitals that prioritize transparency-driven strategies are better equipped to:
- Identify and close reimbursement gaps
- Strengthen relationships with payers through informed, collaborative negotiations
- Guide service line development and revenue planning by analyzing reimbursement rates across payers
- Strengthen operational planning and resource allocation with data-driven insights
Contact Intellimed to learn more about how price transparency data can strengthen your rural health care organization’s strategy.
NRHA adapted the above piece from Intellimed, a trusted NRHA partner, for publication within the Association’s Rural Health Voices blog.
 | About the author: As director of health care innovation at Intellimed, Nathan Schnell leads the company’s consulting and analytic support initiatives, helping health care organizations turn complex data into strategic action. With over 15 years of experience spanning analytics, marketing, customer success, and operations, Nathan brings a practical, data-driven lens to solving challenges—including for rural and community health systems looking to enhance their growth strategies. |
